If you are an adult in crisis, please call the 24/7 Adult Crisis Hotline at 904-206-1756.
If you are a teenager or young adult in crisis, an adult with a child in crisis, or a friend of a youth in crisis, please call the 24/7 Youth Mobile Response Team at 904-580-0529.
Please call 9-1-1 immediately if you or your loved one is having a medical emergency.
WHAT IS DRUG ADDICTION?
HOW DOES ONE BECOME ADDICTED?
Science shows us we need to rethink opioid addiction. Addiction isn't a weakness or a personal failure. It is a disease that hijacks and physically changes the brain, driving people to put the drugs above everything else.
Opioid addiction is a Substance Use Disorder. It is not a moral weakness; it is a chronic disease called Opioid Use Disorder (OUD). It changes and rewires the brain, making it hard for people to quit, even when addiction is destroying their lives. Even when they try again and again.
Like other addictions, opioid addiction happens when a biological system in our brains, the Reward System, is hijacked by opioids. The Reward System drives us to repeat natural things we enjoy, or need to do to survive, like eating when we're hungry. This triggers the release of a chemical called dopamine in the brain, which "rewards" us with a sense of calm or pleasure. But these natural levels of dopamine and their effect can't compare to what is experienced when using opioids.
After time, the brain may be rewired, needing this higher level of dopamine. In fact, over time the brain requires more and more dopamine just to feel "normal."
Once the brain has been rewired by opioids, a person may feel trapped in a continuous cycle. Because OUD is a chronic medical disease, it's a long-term process to help the brain recover. It takes time without using illicit opioids to stop craving them and be satisfied with natural levels of dopamine again.
Anyone who takes prescription or non-prescription opioids can become addicted to them. Nationwide data bears this out.
As many as one in four patients receiving long-term opioid therapy in a primary care setting struggles with opioid addiction, and in 2016, more than 11.5 million Americans reported misusing prescription opioids in the past year.
ROOT CAUSES OF OPIOID ADDICTION
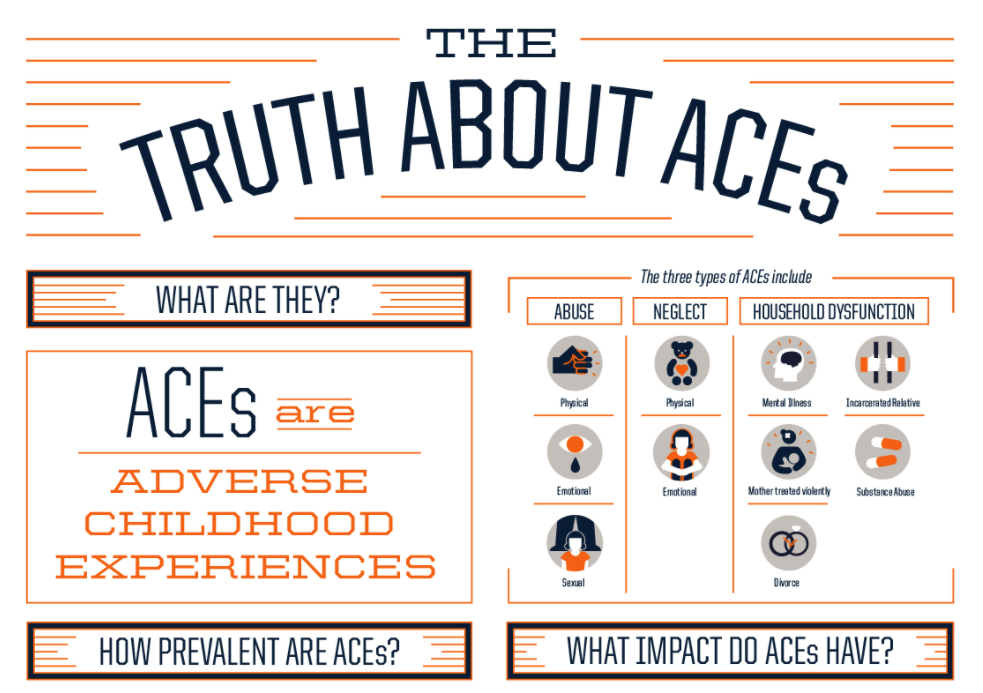
Life experiences, particularly experiences in childhood, have a substantial impact on future physical and mental health behaviors and outcomes, including opioid use.
The landmark 1998 ACE Study investigated the long-term effects of the Adverse Childhood Experiences (ACEs) of abuse, neglect, and household dysfunction and the impacts of these on the physical, mental and social-emotional wellbeing. The study tied childhood trauma directly to an increased rate of opioid use, both among youths and adults. Conducted by Kaiser Permanente and the Centers for Disease Control and Prevention (CDC), researchers surveyed more than 17,000 (largely middle class, educated and white) patients on ten ACEs occurring before age 18 spanning three domains as well as an array of physical, mental and social health issues from patients’ adolescence to adulthood.
Compared to other people who use substances, those who misuse prescription opioids are more likely to report a history of trauma. They also report experiencing trauma at a younger age and are more likely to report ACEs, such as childhood abuse or neglect, or to report having witnessed violence.
The ACE Study highlighted two key findings about substance use. First, parental alcohol and drug misuse was very common—of the 17,000 patients surveyed, 26.9% reported substance abuse in the home during their childhood. (38% percent of opioid users have a close family member who used drugs.) Second, childhood adversity was associated with an increased risk of substance misuse later in life.
As such, the opioid epidemic acts as both a source and outcome of trauma. Those who have a history of trauma also have more difficulty discontinuing opioid use than those with no reported trauma. Watch the video below on YouTube for more information on how Adverse Childhood Experiences affect health across a lifetime.
Intergenerational exposure to trauma plays a key role in opioid misuse—families who have suffered for multiple generations under systemic oppressions such as poverty, community violence and racism, are more likely to report drug use—an attempt to self-soothe in the face of enormous stress and pain.
Those who have a history of trauma also have more difficulty discontinuing opioid use than those with no reported trauma.
THE DISPARITIES OF OPIOID MISUSE
Opioids misuse in the United States occurs more frequently in areas that have experienced high rates of poverty. The largest amount of misuse and overdose death are concentrated in communities with few socioeconomic opportunities.
Additionally, supporting grandchildren impacted by the opioid epidemic can be an added stressor both mentally and financially. As of 2016, an estimated 2.7 million grandparents were raising their grandchildren in the United States, up 7% since 2009, and the AARP attributes this increase to the opioid epidemic.
While opioid misuse is present in all demographics, there are significant disparities in the outcomes of White opioid misuse versus that of Black and Latino misuse. This disparity is evident when examining the death rate due to opioid overdose. To make matters worse, drug use that is seen as a medical condition in White communities is often treated like a criminal act in Black ones. Click here for more information on the disparities among drug enforcement